Abstract
Background: High-dose melphalan with autologous stem cell transplantation (AHCT) is a key component in the treatment of patients with multiple myeloma (MM). The use of AHCT has been shown in several clinical trials to improve event-free and overall survival and is accepted as standard of care in medically fit patients. The use of high doses of melphalan is associated with a period of myelosuppression which has not been reduced despite higher doses of infused stem cells and stem cell fractionation. This period of obligate neutropenia results in significant life-threatening complications and increased financial costs. The aim of this study was to identify predictors of duration of neutropenia as a baseline to developing strategies that minimize neutropenia and thereby symptom burden after high-dose chemotherapy and AHCT.
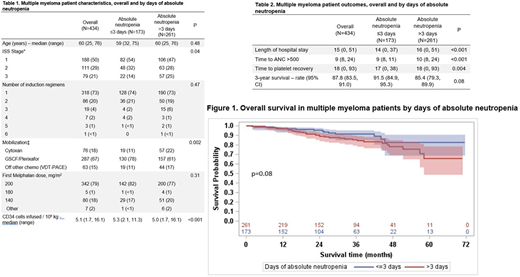
Methods: We retrospectively reviewed patients who had a diagnosis of MM and who had a first AHCT at our Institution between 1/2011 and 12/2016 with high-dose melphalan. We determined the incidence of absolute neutropenia (defined as ANC <500 cells/μL) lasting greater than 3 days. Kaplan-Meier and log-rank test was used to determine overall survival (OS) in patients with neutropenia lasting greater than 3 days or 3 days or fewer. Univariate analysis was done to determine the relative risk of absolute neutropenia greater than 3 days based on age, gender, International Staging System (ISS), cytogenetic risk category, and stem cell dose.
Results: Of 434 patients, 261 (60%) developed absolute neutropenia lasting greater than 3 days (range 4-18). The median age at time of AHCT was 60 years (range) with 188 (50%) being ISS-I, 111 (29%) ISS-II, and 79 (21%) ISS-III. The majority of patients (73%) had 1 induction regimen prior to AHCT. Conditioning was melphalan 200 mg/m2 (79%), 180 mg/m2 (1%), or 140 mg/m2 (18%). The median cell dose was 5.1 x106 CD34+ cells/kg (range 1.7-16.1). Patients with absolute neutropenia lasting greater than 3 days had longer hospitalizations (p=<0.001), longer time to ANC recovery (p=<0.001), and longer time to platelet recovery (p=0.004) compared to patients who had absolute neutropenia for 3 days or less. With a median follow up of 30 months (range 3- 72), 50/434 had died for a 3-year OS of 87.8% (95% CI: 83.5- 91.0). The 3-year OS for patients who had absolute neutropenia greater than 3 days was 85.4% (95% CI: 79.3 - 89.9), compared to 91.5% (95% CI: 84.9 - 95.3) for patients who had absolute neutropenia for 3 days or fewer. There was a trend towards improved survival in patients with absolute neutropenia lasting 3 days or fewer (p=0.08). By univariate analysis, patients with ISS stage III disease had an increased risk of greater than 3 days of absolute neutropenia compared to patients with ISS stage I (RR: 1.28, 95% CI: 1.06 - 1.54; p=0.009). Patients who received fewer than 4.25 x 106 CD34+ cells/kg had an increased risk of greater than 3 days of absolute neutropenia compared to patients who received greater than 6.06 x 106 CD34+ cells/kg (RR: 1.59, 95% CI: 1.27-1.98; p<0.001).
Conclusions: The incidence of obligate absolute neutropenia lasting 3 days or more was 60% in patients after high-dose melphalan AHCT and duration of neutropenia impacted post-AHCT outcomes. While there was no statistical difference in OS in patients with less or greater than 3 days of neutropenia, there was a trend towards better survival in patients with absolute neutropenia of 3 days or less. To our knowledge this is the largest series in the modern era to report on engraftment kinetics after AHCT in MM patients. Minimizing the duration of neutropenia and need for transfusion support during AHCT has the potential to improve the safety of high-dose therapy, reduce costs, and decrease transplant-related morbidity and mortality.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal